Skin Cancer Treatment Options at the Rehoboth Plastic, Derm Center and Medispa
 Preventing Skin Cancer Solutions
Preventing Skin Cancer Solutions
Our skin cancer center is designed to treat basal cell carcinoma, squamous cell carcinoma and melanoma since these three skin cancers make up over 99% of all skin cancers diagnosed in the U.S. The best way to prevent and treat skin cancer is to focus on prevention and early detection. Skin cancers are easier to treat and have a much higher rate of cure when detected earlier.
Treatment for basal cell carcinoma and squamous cell carcinoma
When weighing the pros and cons of all the different treatment options, it’s important to understand that nonsurgical treatments plus curettage and electrodessication all have one significant drawback in common – no tissue is examined under the microscope, therefore there is no way if you know if the cancer was completely removed.
In our skin cancer center, surgical treatment of skin cancer using immediate microscopic margin controlled removal (modified frozen section technique) remains the standard of care as long as it is safe, effective (99% success rate) and cost effective.
Skin cancer is an abnormal growth of skin cells that most often develops on areas of the skin exposed to the sun’s rays. Skin cancer tends to affect people mostly with light skin who sunburn easily.

Dermatologic surgery – Squamous cell carcinoma, right hand treated with plastic surgery removal with microscopic margin control and skin graft.
Dr. Chang is a great doctor with a warm bedside manner. He takes care of my family with routine skin checks and knows how I need to be reassured that all will be ok. When I had melanoma on my face, it was comforting to know that he was also a plastic surgeon. He gave his advice for the best closure. His staff is wonderful as well. I highly recommend him.
What is the most important message on what you can do in “PREVENTING SKIN CANCER”?
- Focus on what YOU can control
- Prevention = sun protection
- Early detection
- Comprehensive skin cancer care and melanoma center: skin screenings, skin spot consultations, biopsies, nonsurgical treatments, skin cancer removals (all types), skin cancer prevention, treatment of precancerous skin lesions (actinic keratoses, dysplastic nevus), removal benign skin lesions and tumors
- Providing skin cancer care across Delaware and Delaware Valley: Newark, Rehoboth Beach, Dover, Delaware
- Skin cancer (basal cell and squamous cell carcinoma) removal and immediate closure in office under local anesthesia; microscopic margin controlled removal using modified Frozen Section/Mohs technique with 99% success rate (>1600 consecutive frozen section procedures); >5000 skin cancer removals over 20 years experience
- Dr Lawrence Chang, board certified plastic surgeon specializing cosmetic, reconstructive and dermatologic surgery and cosmetic medicine; founder and medical director
- Johns Hopkins University/ University of Pennsylvania trained
- Top Doc Philadelphia Magazine and Delaware Today Magazines Plastic, Cosmetic and Dermatologic Surgery
- Plastic and Dermatologic Surgery teaching site for Christiana Care General Surgery residency program, multiple Physician Assistant Programs- Arcadia, Jefferson, Drexel, PCOM
-
What is skin cancer?
Skin cancer is an uncontrollable growth of abnormal cells in the epidermis, the top layer of skin, caused by sun exposure and the use of UV tanning beds. People with a skin cancer will unknowingly call them a “bump”, “pimple” or “sore that won’t heal”.
The sun’s harmful ultraviolet (UV) rays cause unrepaired DNA damage that triggers mutations to normal cells (basal cells, squamous cell, melanocytes, Merkel cells) in the outermost skin layer. These mutations in these skin cells lead to rapid growth of these cells forming malignant tumors. The main types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma which represent the vast majority of skin cancers seen and treated at our skin cancer center.
Less commonly seen are Merkel cell carcinoma (MCC), lymphoma of the skin and Kaposi sarcoma.
Skin cancer is the most common form of cancer with 1 out of 5 Americans developing skin cancer by age 70. The good news is if your skin cancer is detected early, your doctor can treat it with high degree of success.
-
What are the types of skin cancer
- Basal cell carcinoma (BCC): Most common form of skin cancer that arises from the skin’s basal cells with > 4 million cases diagnosed in the U.S. each year. BCC most often found on sun exposed areas of the body, especially face, neck, ears, scalp, arms, legs, back and shoulders. This skin cancers rarely spread and are rarely fatal however, if untreated can be locally destructive.
- Squamous cell carcinoma (SCC): The second most common skin cancer that arises from the skin’s squamous cells with > 1 million cases diagnosed in the U.S each year. Found on sun exposed areas of the body and can sometimes grow rapid and spread if not detected and treated early. Up to 15,000 deaths from invasive SCC reported in the U.S. each year.
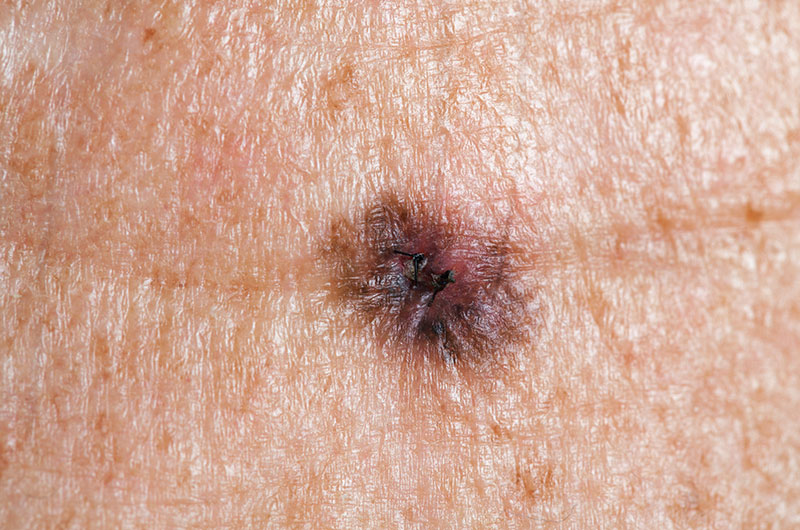
- Malignant melanoma: Is the most dangerous of the three most common forms of skin cancers arising from melanocytes, the skin cells that produce melanin which gives skin its color. Melanomas look like moles either brand new or changing appearance and will show up throughout the body even in areas not exposed to the sun. In 2019, >192,000 new cases of melanoma are diagnosed with over half will be invasive. Melanomas can be curable when detected and treated early. In 2019, melanoma is projected to cause approximately 7,200 deaths. What is most concerning is that melanoma is common in people under the age of 30 years and one of the most common cancers found in young people today (especially young women).
- Merkel cell carcinoma (MCC): Is a rare, aggressive skin cancer arising from skin cells associated with sensory nerve endings. These firm painless bumps appear in sun exposed areas of the body in fair skin individuals over the age of 50. MCCs are at high risk for metastasizing and recurring, therefore early detection and treatment are crucial.
- Lymphoma of the skin (CTCL): It is a rare type of cancer that starts in your white blood cells (T cells) of the immune system that develops abnormalities and begin to attack your skin. CTCL often resembles eczema or psoriasis and appears as rash like skin redness, slightly raised or scaly patches and some small bumps or tumors on the skin. The treatment is nonsurgical and includes skin creams, light therapy, radiation therapy or chemotherapy.
- Kaposi sarcoma (KS): It is a cancer that develops from cells that line the lymph or blood vessels. These abnormal cells form purple, red or brown blotches or tumors on the skin often appearing on the legs or face. KS can cause serious problems or be potentially life threatening when they involve the lungs, liver or digestive tract and usually referred to medical oncology for comprehensive management
-
What are the types of precancerous skin lesions?
Actinic keratoses and dysplastic nevus are the two most common precancerous skin lesions treated at our skin cancer centers. If left untreated, a small percentage of these abnormal lesions can eventually become skin cancer. The best way to prevent skin cancer is proper screening, early detection and when indicated, treatment of some of these precancerous lesions.
Actinic Keratoses (AKs)
- What are they? These are rough, dry scaly patch of skin, usually <1 inch diameter, pink,brown or red and in some cases a hard wart like surface usually found on sun exposed areas of the face and body.
- Do they need to be treated? Yes. If left untreated, it has been reported that up 10% will eventually become squamous cell carcinoma.
- What are the treatments for AKs?
- Medications: Fluorouracil cream (Efudex, Carac), Imiquimod (Aldara, Zyclara), Igenol mebutate gel (Picata), Diclofenac (Voltaren, Solaraze). These creams may cause redness, weeping, scaling or burning sensation for a few weeks
- Freezing (cryotherapy): most common treatment using liquid nitrogen to create a very superficial burn to the skin causing the lesions to slough off and new skin to appear. Side effects include blisters, redness, scarring, pigment art changes.
- Scraping (curettage)
- Photodynamic therapy
Dysplastic Nevus (DN)
- What are they? They are abnormal or atypical moles that are larger and irregular in shape than an average mole (>6mm). DN have uneven colors with dark brown centers and lighter uneven edges. These moles tend to be hereditary. In Caucasian individuals in the US, the lifetime risk of developing melanoma is less than 1%, whereas in patients with dysplastic nevi, the risk is greater than 10% and this rises to over 50% in people with family history of dysplastic nevus syndrome.
- Do they need to be treated? The treatment of dysplastic nevi is controversial and varies from provider to provider especially when the biopsy of the abnormal mole reveals “mild to moderate” abnormal cells since the likelihood of melanoma is extremely low. It is universally agreed that a dysplastic nevus with severe atypia or one that cannot be distinguished histologically from melanoma should be reexcised with a clear margin.
- What is the treatment for dysplastic nevus?
- Surgical removal for dysplastic nevi with moderate to severe atypia
- Controversial for mild to moderate dysplastic nevus
- Annual screenings with body photography and monthly self examinations
-
What should I expect at my skin screening/ skin spot check/ skin cancer consultation?
- People come to our skin cancer for one of the following concern(s): 1. routine skin screenings without any concerns; 2. high risk patients with or without previous skin cancers requesting skin screening; 3. patient with a suspicious lesion they note as a bump, pimple or sore that won’t heal; 4. patient with a biopsy positive skin cancer for treatment
- Evaluation of general medical conditions, medications, allergies, previous skin cancers or precancerous lesions and treatments, sunburn history, previous surgeries, exposure to smoking, family history skin cancer
- Examination of skin lesion(s) of question or head to toe full body scan
- Body or spot photography
- Discussion of treatment options: 1. Observation, education on prevention techniques, 2. Biopsy if indicated, 3. Treatment of suspected precancerous lesions, 4. If biopsy proven skin cancer, options for treatment discussed (surgical and nonsurgical)
- Discussion of surgical treatment of skin cancer removal
-
What are the risks of a skin cancer removal procedure?Bleeding, infection, poor healing along incisions, scars, recurrent cancer, numbness, pain
-
What should I expect at my skin cancer removal procedure?
- Your skin cancer removal procedure is performed in the office setting under local anesthesia with the average time for cancer removal, microscopic examination and surgical closure is approximately one hour
- You may have a light meal before your procedure
- Do not take any aspirin or blood thinners 7-10 days prior to procedure. Any critical blood thinners for heart condition may be continued up to the time of the procedure
- Bring a driver and wear loose comfortable clothing
- Prior to your skin cancer removal, your pathology results will be reviewed, your skin cancer is site identified and confirmed by the patient and the surgeon, the visible borders of the skin cancer is marked with a marking pen and photographs are taken
- A local anesthetic is injected to numb up the area and the area is cleansed with surgical soap
- The skin cancer is removed with a scalpel blade taking a small 1 mm rim around the entire perimeter of the tumor. The 12 o’clock border is marked for analysis by the pathologist. This is the Stage 1 removal.
- The pathologist will process the skin cancer using a modified Frozen Section/ Mohs Technique to accurately determine if all the cancer cells have been removed
- If there are no more cancer cells on the microscopic analysis, the surgeon will proceed to closure the defect with sutures. If there are cancer cells still present, additional margins are taken where appropriate for further analysis until all the cancer cells have been removed
- After final closure, a dressing is applied and discharge instructions are given
- The choice of surgical closure depends on the amount of available skin and location of the skin cancer. If there is sufficient skin available, there will be a straight line scar closure. If there is a lack of available local skin, there with be a and local flap closure that will leave a zig zag or curved scar closure. If there is no available tissue to use as a local flap, a piece of skin taken from another area that has ample skin will be used as a skin graft. The final choice of closure technique is based upon what is best to allow safe, predictable healing with avoiding functional distortion and best possible esthetic outcome
- Skin cancer treatments on the legs have the most difficult time healing and require a minimum of 1 week of careful and thoughtful elevation. If a skin graft is used, an additional 2 weeks of elevation with ace wraps may be required
- Scar management as be started a couple of weeks after suture removal and stable healing of the incision. This might include topical vitamin E or silicone gel.
- Patient should continue to have annual skin screenings and as needed visits for any new skin lesions of concern
NONSURGICAL
- Cryotherapy
- Photodynamic therapy
- Topical chemotherapy: 5-fluororacil (Efudex, Carac) apply 1-2x a day up to 4 weeks, most severe skin reactions; Dicofenac (Solaraze) apply twice a day 2-3 months; Ingenol mebutate (Picata) apply once a day for 2-3 days
- Immune response modifiers: Imiquimod (Zyclara) apply few times a week for several weeks, severe skin reactions, flu like symptoms; Interferon
- Laser surgery
- Chemical peels
- Radiation therapy: large tumors, multiple cancers (cancer field), not surgical candidate
- Systemic chemotherapy: if squamous cell carcinoma has spread
- Targeted therapy: drugs different from chemotherapy
- Immunotherapy: advanced squamous cell carcinoma not treatable with surgery or radiation therapy
SURGICAL
- Curettage and electrodessication: skin cancer is scraped off with a sharp tool under local anesthesia, then heat is used to destroy remaining cancer cells and stop any bleeding. For small skin cancers, a white round scar is left behind. 95% successful
- Excision: entire skin cancer is removed under direct visualization with a “safety margin”, closed with sutures and sent to an off-site lab for analysis with a <5% chance that there may be cancer cells left behind that might require more removal. 95+% successful.
- Modified frozen section/Mohs technique (intended for physician education): In office procedure performed under local anesthesia with immediate microscopic margin controlled surgical removal of the skin cancer in stages. 1. For the stage 1 removal, the surgeon will mark the visible perimeter or the skin cancer with a marking pen, 2. Local anesthesia is given and the surgical site prepped and draped with surgical soap, 3. 1mm thin margin is cut with a scalpel blade and beveled outward at a 45 degree angle to give an additional 1-2 mm peripheral margin and down through the depth of the dermis not disturbing the underlying fat, 4. The skin cancer specimen is marked for orientation for microscopic pathological determination, 5. Microscopic examination: a modified frozen section technique is used by inking all peripheral and deep margins with different colors to maintain proper orientation for skin cancer margin analysis. A “CURVED bread loaf” technique (“SHOM” technique) of processing the skin cancer specimen so that every edge of the skin cancer will be microscopically examined similar to the Mohs technique. The main advantage that the modified frozen section technique has over the Mohs technique is having the entire skin cancer on the microscopic slide when examining all margins for any remaining skin cancer cells. This allows the pathologist to more accurately assess whether the true margins are free from cancer cells and keep the final defect as small as possible. The main disadvantage of the Mohs technique is the skin cancer is NOT entirely on the slide and therefore it may be difficult to assess if the margin is free of skin cancer which sometimes results in false positive readings on the margins and a larger Mohs defect compared to the modified frozen section technique (frequently seen in people with sebaceous glands that creates potentially confusing microscopic “artifacts” in the skin particularly face, cheek and nose), 6. If the microscopic margins are free of cancer cells, the plastic surgeon will close the defect using the appropriate closure method, 7. If the microscopic margin has residual cancer cells, additional tissue is removed based upon where there is remaining cancer and sent as another stage for microscopic analysis. This process is repeated until it has been determined that all cancer cells are removed, 8. After closure of the skin cancer defect, a dressing is placed and discharge instructions are given

Treatment of Melanoma: is based upon the stage of the melanoma which is determined from the initial biopsy of the abnormal lesion
- Treatment early melanoma (stage 0 noninvasive, stage 1)
- Melanoma in situ (stage 0): cancer localized to outermost layer of skin, the epidermis
- Stage 1 melanoma: cancer cells invade the second layer of skin, the dermis
- Stage 0 and stage 1 melanoma treated by surgery where the tumor is removed with a “safety margin” of normal tissue to a certain margin both around the perimeter and depth. The amount of normal skin removed depends upon the initial thickness and location of the melanoma. If the final margins are cancer free at a certain distance, no further surgery is needed. Many of these early melanomas could be surgically removed in the office setting under local anesthesia but the patient would be offered the ability to have anesthesia for their procedure.
- Depending on each case based upon appearance and location of the melanoma, the surgical plan could be: 1. Standard removal of a preset margin and immediate closure, 2. For melanomas of the face and scalp, a staged removal with preset margins, temporary dressing placed and return back 3-7 days for surgical closure after permanent pathological analysis of margins are determined, 3. Modified Frozen Section/Mohs removal of the tumor and immediate closure after all margins determined to be clear
- If melanoma measures more than 1.0 mm in thickness or has ulceration or high mitotic rate, a lymph node biopsy (Sentinel lymph node biopsy) will performed which scheduled under general anesthesia
- Genetic testing of the tumor is also recommended to assist in determining the likelihood of recurrent cancer or spread of the cancer
- Treatment intermediate, high risk melanomas (Stage 2)
- Since risk of tumor spread to lymph nodes is higher in stage 2 melanomas, a sentinel lymph node biopsy is performed at the same time of melanoma removal. If cancer cells is found in the sentinel node, you might need the rest of the lymph nodes in the area removed to determine the presence of anymore cancer cells
- After surgery, referral to medical oncologist to determine if additional treatment would be required such as immunotherapy
- Treatment advanced melanoma (Stage 3,4)
- Advanced melanomas that have spread beyond the original tumor into lymph nodes or distant organs make them difficult to treat
- Referral to medical oncology would facilitate the possibility of other adjuvant therapies with the advent of pioneering breakthroughs in immunotherapy
Dr. Chang squeezed me in unexpectedly last week for a Mohs surgery due to the other surgeon having an emergency. Really loved his bedside manor and pleasant demeanor which kept me calm and at ease. The staff was great, too and the procedure was over before I knew it! The nurses also took the time to explain the discharge instructions and after-care. Would highly recommend!

 Skin Cancer Removal
Skin Cancer Removal Skin Cancer Closure
Skin Cancer Closure